Tracheostomy tubes play a critical role in patient care, particularly for individuals requiring long-term airway management or mechanical ventilation. Selecting the appropriate tracheostomy tube can significantly impact patient comfort, recovery, and overall outcomes. This article provides a comprehensive guide to help healthcare professionals choose the right tracheostomy tube for their patients by considering factors such as patient needs, tube materials, sizes, and specific clinical conditions.
Understanding Tracheostomy Tubes
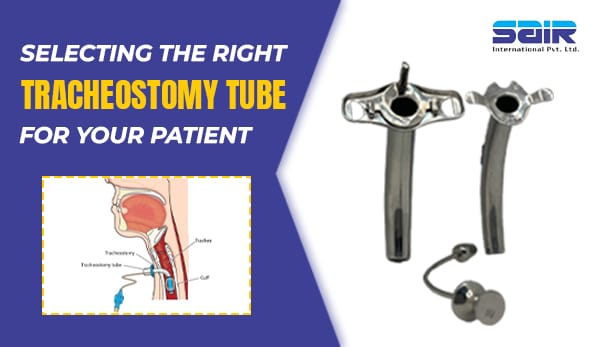
A tracheostomy tube is inserted into a surgically created opening in the trachea to establish a direct airway. It facilitates breathing, allows for mechanical ventilation, and assists in clearing secretions. These tubes come in various designs, materials, and configurations to accommodate different patient requirements.
Key Components of a Tracheostomy Tube
- Outer Cannula: The main tube that maintains the tracheal opening.
- Inner Cannula: A removable insert within the outer cannula, allowing for easy cleaning and maintenance.
- Cuff: An inflatable balloon at the distal end that seals the airway to prevent aspiration and improve ventilation.
- Flange: The external plate that secures the tube and provides stability.
- Obturator: A guide used during insertion to prevent tissue trauma.
Factors to Consider When Selecting a Tracheostomy Tube
1. Patient Anatomy
- The patient’s age, neck length, and tracheal diameter are essential factors in selecting the appropriate tube size and design. Pediatric patients require smaller tubes, while adult patients may need customized options for unique anatomical variations.
2. Cuffed vs. Uncuffed Tubes
- Cuffed Tubes: These tubes are equipped with an inflatable cuff that seals the airway, making them suitable for patients on mechanical ventilation or at risk of aspiration.
- Uncuffed Tubes: Ideal for patients who can breathe independently and have a low risk of aspiration, uncuffed tubes allow for natural airflow through the upper airway.
3. Material Composition
- PVC (Polyvinyl Chloride): Lightweight and cost-effective, PVC tubes are commonly used for short-term applications.
- Silicone: Soft, flexible, and hypoallergenic, silicone tubes are preferred for long-term use due to their patient comfort.
- Metal: Durable and reusable, metal tubes are suitable for patients requiring permanent tracheostomies.
4. Tube Size
- The internal diameter (ID) and external diameter (OD) must match the patient’s airway dimensions to ensure proper fit and functionality.
- Over-sizing can cause trauma or discomfort, while under-sizing may result in inadequate ventilation.
5. Fenestration
- Fenestrated Tubes: These tubes have small openings to allow airflow to the vocal cords, enabling speech.
- Non-Fenestrated Tubes: Suitable for patients who do not require vocalization or have significant aspiration risk.
6. Duration of Use
- For temporary airway management, disposable tracheostomy tubes are practical and hygienic.
- Reusable tubes are cost-effective for long-term patients, provided they are adequately cleaned and maintained.
Special Considerations for Specific Patient Groups
Pediatric Patients
- Pediatric tracheostomy tubes are smaller and lack cuffs to minimize airway trauma.
- The tube material should be soft and flexible to accommodate sensitive pediatric anatomy.
Patients with Complex Medical Conditions
- Patients with tracheomalacia or other structural abnormalities may require custom-designed tubes.
- For patients undergoing radiation therapy or with neck deformities, flexible or adjustable-flange tubes are ideal.
Patients Requiring Speech
- Speech valves, such as Passy-Muir valves, can be attached to fenestrated tubes to enable phonation.
- Collaborative care with speech therapists is essential to optimize communication.
Guidelines for Proper Sizing and Placement
- Measure the Airway: Use imaging techniques or anatomical assessments to determine the appropriate tube size.
- Choose the Right Length: Consider the patient’s tracheal length to avoid complications like mucosal irritation or improper positioning.
- Confirm Placement: Always verify the tube’s position with imaging or endoscopic guidance.
Managing Patient Comfort and Safety
- Monitor for Complications:
- Regularly assess for signs of infection, tube displacement, or airway obstruction.
- Evaluate cuff pressure to prevent tracheal damage.
- Educate the Patient and Caregivers:
- Provide clear instructions on cleaning and maintaining the tube.
- Teach caregivers how to recognize early signs of complications.
- Ensure Adequate Humidification:
- Use humidifiers or heat-and-moisture exchangers to prevent drying of the airway.
Conclusion
Selecting the right tracheostomy tube is a critical component of patient care. By considering factors such as patient anatomy, medical condition, and specific clinical needs, healthcare providers can optimize outcomes and improve the patient’s quality of life. Collaboration with multidisciplinary teams, including respiratory therapists, speech therapists, and surgeons, ensures comprehensive and patient-centered care. Ultimately, a well-chosen tracheostomy tube not only supports respiratory function but also enhances comfort, communication, and overall recovery.